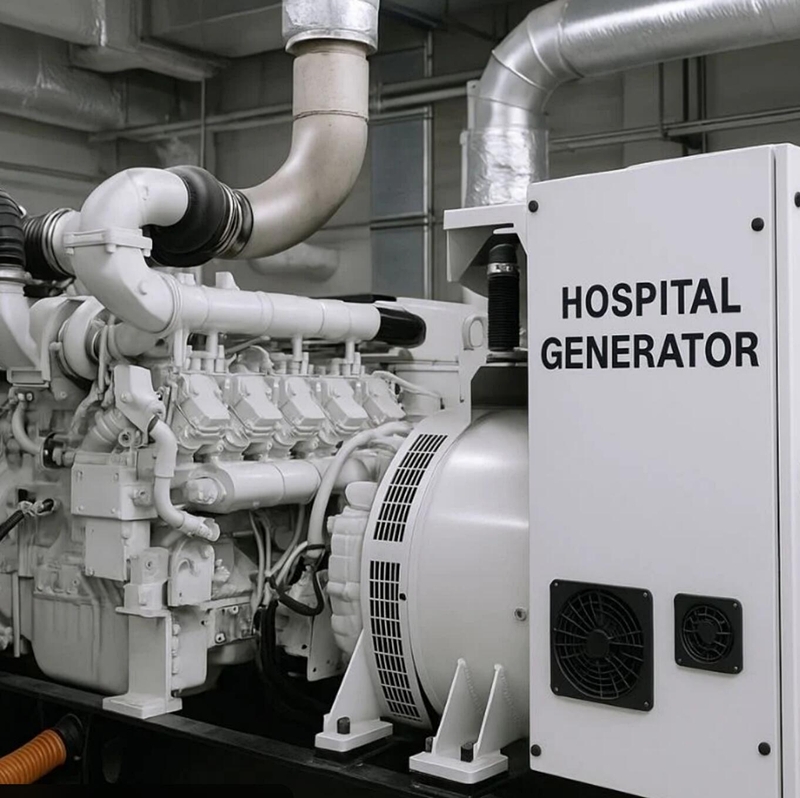
A backup generator is not optional for hospitals. It is a life-safety system. Without a properly designed emergency power system, a hospital cannot operate safely during a grid failure. Even short power interruptions can affect life-support equipment, operating rooms, oxygen systems, and critical care units.

Why Hospitals Cannot Afford Even a Short Power Loss
In most commercial buildings, a 10–20 second outage is inconvenient.
In a hospital, those same seconds can interrupt:
- ICU ventilators
- Operating room equipment
- Oxygen supply systems
- Emergency lighting
- Nurse call systems
- Blood storage refrigeration
Hospitals are not designed around “if power fails.” They are designed around “when power fails.”
That difference alone explains why emergency power is treated as core infrastructure.
A Hospital Generator Is Not Just a Bigger Standby Unit
One of the most common misunderstandings I see is treating hospital generators as oversized commercial standby units.
That approach usually leads to underdesign.
In real projects, hospital installations often require:
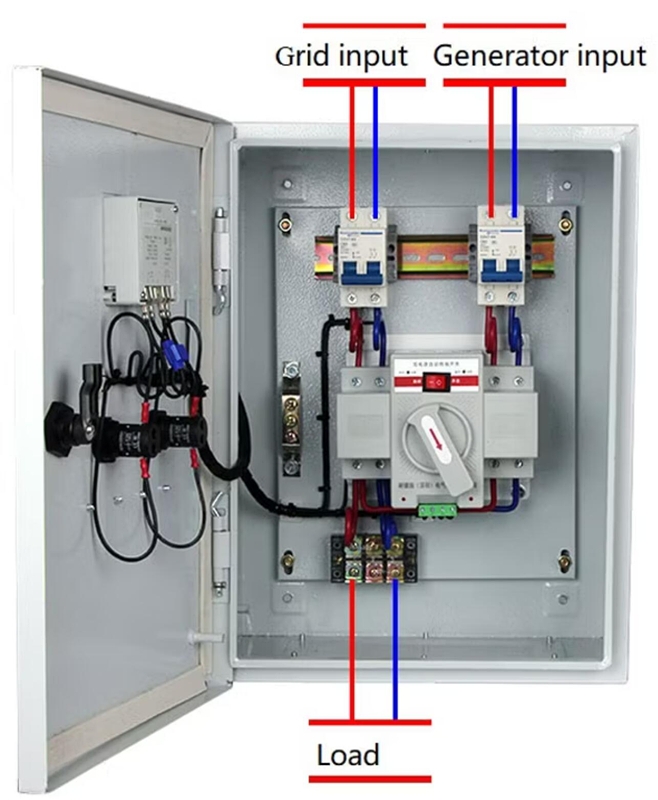
- Automatic Transfer Switches (ATS)
- Separation of life-safety and non-critical loads
- Dedicated emergency distribution panels
- Sometimes dual generators operating in parallel
- Fuel systems designed for extended operation
I’ve seen cases where buyers initially requested a single large generator, only to later realize that redundancy and synchronization were necessary.
In medical facilities, a single point of failure is unacceptable.
The Most Common Procurement Mistake
The biggest mistake is focusing only on rated kVA.
Generator size alone does not determine system reliability.
What actually matters is:
- Load prioritization strategy
- Transfer timing
- Expected annual operating hours
- Redundancy planning
- Fuel autonomy duration
- Maintenance accessibility
A hospital generator is not just about starting during an outage.
It must sustain stable operation under worst-case conditions.
Prime Power vs Standby Power - Often Confused
In regions with unstable grids, hospitals may rely on generator power frequently.
If the unit operates daily or for extended periods, selecting a standby (ESP) rating purely to reduce cost can create long-term reliability problems.
When reviewing medical projects, I always ask:
How many hours per year will this generator realistically run?
If the answer is unclear, the configuration decision is already at risk.
Choosing rating based only on price is one of the most common causes of premature wear and overload shutdowns.
What Happens If the System Is Undersized?
From what I’ve observed in export projects, poor design decisions can result in:
- Voltage instability affecting sensitive equipment
- Overload during peak demand
- Fuel shortages during extended outages
- Lack of backup if one unit fails
In a retail building, these are operational disruptions.
In a hospital, they are safety risks.
That is why conservative design is often justified in healthcare environments.
Is One Generator Enough for a Hospital?
For small clinics with limited loads, a single properly sized standby generator may be adequate.

For medium and large hospitals, I rarely recommend:
- A single unit without redundancy
- No synchronization capability
- No structured maintenance planning
In high-risk environments, hospitals effectively operate like small power plants.
The emergency power system should reflect that operational reality.
Conclusion
A backup generator in a hospital is not an accessory system. It is part of the life-protection infrastructure.
Underdesigning a hospital generator system creates risk that only becomes visible during failure. And in medical facilities, failure is not just a financial issue - it can directly impact patient safety.
When evaluating hospital power systems, I prefer conservative design over minimal compliance. In healthcare applications, underdesign is more dangerous than overspecification.
If you are reviewing a generator configuration for a medical facility, define load priority, realistic operating hours, and redundancy requirements before selecting capacity. Those three factors determine whether the system will perform when it is truly needed.